Osteoarthritis of the knee

Hello and welcome to our winter edition. This newsletter will revisit knees and osteoarthritis (OA). Reason being, we are frequently asked about knee joint pain and there are still many misconceptions out there. Many people are under the impression that nothing can be done for OA knees.
We will look at different types of osteoarthritis and knee joint pain. Two common types of OA include non-traumatic OA and post traumatic OA. We will look at how these come about and possible management of them.
Our usual exercise page is included and of course this will concentrate on strengthening the muscles around the knee.
Don’t forget to let us know if there are any topics that you would like us to discuss in future editions.
Non traumatic vs Post traumatic knee joint pain
Traumatic OA may occur in younger people, often before the age of 40 years of age. It is usually the result of an injury involving their knee joint. We find that this group often have symptoms on the outside of the knee and often involve the kneecap (patella).
Non traumatic OA of the knee usually happens gradually over time without a specific episode of injury or trauma. It is most common in the over 70 years age group. In this group often most of their discomfort occurs on the inside of the knee. This group also commonly show a change in the way they walk and move. For example, commonly a patient will walk with their upper leg turned inwards and the knee bending inwards. This places a lot of compressive pressure on the outside and a stretching force on the inside of the knee.
When we treat patients who come in with arthritic changes there is a lot to address and work on before surgery should even be considered. Correcting walking patterns which may include strengthening of muscles, stretching of others, as well as educating you about why you may have knee joint pain and what you can do about it.
Anatomy of the knee joint
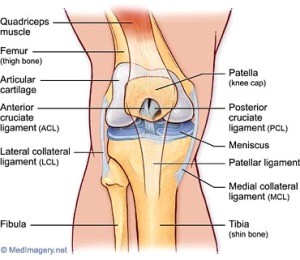
The knee joint includes the femur (thigh bone) and tibia (shin bone) and the patella (kneecap). There is the meniscus (cartilage) in between the femur and tibia that provides a nice sitting space for the femur to sit on the tibia. There is also cartilage found at the end of the long bones (femur and tibia) and behind the patella.
All these different structures may be affected by the process of OA. There may be some deterioration in the cartilages or at the end of the bones.
What can be done for OA?
Many people make the mistake of thinking that nothing can be done for the structural changes mentioned above. Many studies have been done that indicate what we find on X-rays, MRI etc do not always reflect what a person’s symptoms are. I have seen many many X-rays that state ‘bone on bone’ however the patient does not indicate they have any pain in this area.
There may be other changes causing knee joint pain or a change in functional ability. These may be due to changes in muscle strength and flexibility. With pain there is often a subconscious protective reflex so that the surrounding muscles weaken or get stiffer. Treatment would therefore focus on strengthening and stretching these muscles.
When a patient comes in for knee pain we assess these muscles to see whether there is a deficit that we can address and help restore. We also look at the patellofemoral joint of the knee. This joint is between the patella and femur as the name suggests. This joint is susceptible to changes in muscle strength, namely weakness of thigh muscles which lead to a change in how this joint works which then may cause pain.
We assess how this joint is functioning and if there is a problem, we can address this to maximise how it works which often results in a decrease in pain and an increase in functionality. There are many factors that can influence knee function and pain in the knee.
Case study of a 30 year history of knee joint pain
I am including this case study just to illustrate how someone presenting with preconceived ideas of knee pain can be helped. Patient X an 80 yo male came to see me (because his wife mentioned to me that her husband was having difficulties walking because of knee pain and so she made him come!!). Mr X came and reported a 30 year history of knee pain and an x-ray that showed “bone on bone’, he did not want a knee replacement but now was having significant difficulties walking downstairs and walking.
After examining Mr X his patellofemoral joint was very stiff. His surrounding muscles had also weakened because they had been protected for so long. Treatment addressed both these issues and his pain reduced significantly. He no longer felt he needed a knee replacement and he was able to walk downstairs pain free and increase his walking.
The exercises include strengthening exercises for the quadriceps (thigh muscles), gluteals (bum muscles) and the calf muscles. All these muscles help provide support for the knee.
They should not cause significant pain in the knee. If there is pain, you may have to decrease the intensity of the exercise. Come in and check your technique if you have any further problems.

